Precision Medicine trespasses into the clinic

Prabhu Sampath
1989 EEE
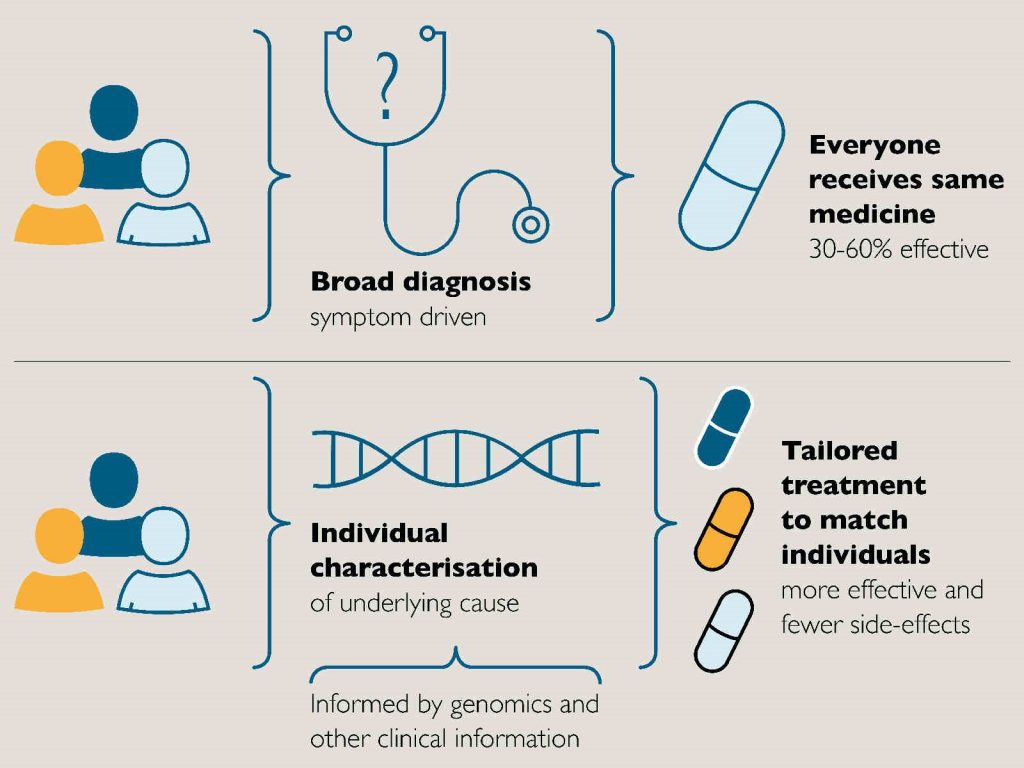
Precision Medicine also referred to as personalized medicine and stratified medicine is finally pushing its way into the clinic with brute force.Precision Medicine is simply taking healthcare from One-Size-Fits-All to Personalized Treatments.
Precision medicine has spent the last decade in discovery and validation. Genetics has given way to Genomics. Genetics and genomics both play roles in health and disease. Genetics refers to the study of genes and the way that certain traits or conditions are passed down from one generation to another. Genomics describes the complete study of all the genes of a person.
The progress was painfully slow despite the disruptive advancements in Next Generation Sequencing (NGS). The extensive research and validation of the NGS results, backed by exponential advances in bioinformatics, have now paved the path for truly translational efforts, changing the game in the way, we treat patients with successful outcomes that we have never seen before.
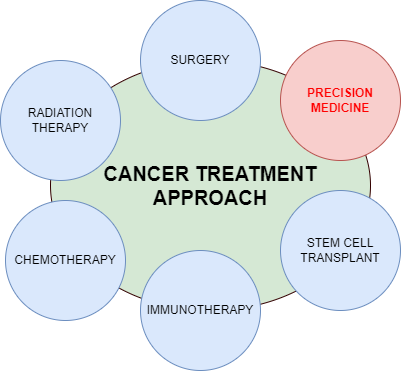
In an ideal world, precision medicine is meant to be used in prevention and treatment approaches for all health issues. We still have a long way to go. Its day-to-day application in most disease states is relatively limited. Despite this, in certain areas of medicine, such as oncology and reproductive health, precision medicine is already routinely put to use.
Precision medicine focuses on three critical aspects that touch on prognosis, therapy, and screening. Despite all three being equally important, early-risk screening facilitates timely intervention and helps prevent or delay the onset of many diseases and manage the condition better.
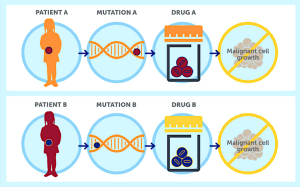
The first is genomic testing referred to as also referred to molecular or genetic testing in the past, and simply focuses on identifying changes in chromosomes, genes, or proteins, that cause disease.
The second aspect is a logical next step to the first. Having found disease-causing changes, efforts are on to design, devise, and deploy targeted therapies, which are drug treatments that interfere with specific molecular targets causing the disease.
The final one is to identify genomic markers, which are genetic elements that convey the risk information or likelihood of an individual acquiring a disease. The earlier aspects look for changes in a diseased condition while the final one focuses on predisposition. This may also give some indication of a prognosis after the onset of a disease.
The biggest bottlenecks that we face in precision medicine today despite all the advances made, are the turnaround times and the prohibitive costs. These tests that began with months to produce results, are turning them around in weeks now. Weeks will need to become days if we have to make an impact and save a patient who is already terminally ill. There is no doubt that this is bound to happen quite soon.
The Covid19 pandemic necessitated the acquiring of one important learning. No technology is appropriate, until it is democratized, and reaches all sections of society. The affordability of detection and therapeutics is a crucial element in early and universal adoption. The plunge in the costs of Real-Time PCR testing, during the pandemic, gave insights that scaling the numbers is key. The rapid development and deployment of vaccines were only possible due to the magnitude of numbers despite the financial burden. The above inference is what we need to enable in precision medicine. Otherwise, this will continue to benefit only a privileged few.
The positive is that both turnaround time and costs are constantly reducing and yet the final destination is far away. There is also an early adoption of limited tests by insurance companies. The more tests covered, the more will precision medicine become more routine.
The constant learning will translate to patients receiving more optimal treatments, targeted to their disease, improving response and decreasing side effects by limiting exposure to drugs that are not effective and getting the best dose for them based on their genomic profile. Thus, patients will live longer with fewer complications from their treatments (e.g., including neuropathies, cardiac toxicity, and others).
The ethical concerns surrounding genomic testing have been addressed to a great extent including misleading results and privacy issues.
The tremendous future value of genomics is clear and far clearer than for other emerging technologies. The countries that make aggressive investments in infrastructure and applications will be positioned to reap the greatest rewards for decades to come.